HAEMORRHOID SURGERY
What are haemorrhoids ?
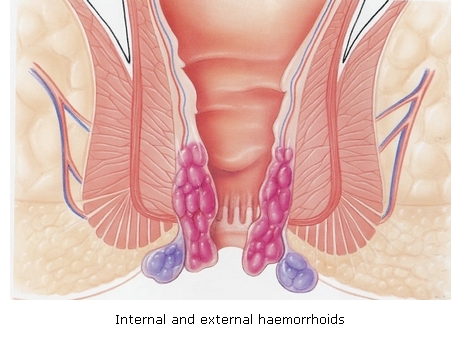
The anus is lined by a dense network of blood vessels that can become congested causing a burning pain during the passage of stools and leaving traces of fresh blood on the toilet paper. Prolapsed haemorrhoids give the feeling of a foreign body between the buttocks and cause soiling. Haemorrhoidal crisis is managed using painkillers, venotropic drugs, laxatives and topical anti-inflammatory agents. Once the crisis is over mild residual internal haemorrhoids can treated endoscopically by banding. More advanced prolapsing disease is only amenable to surgery which involves vessel ligation and removal of prolapsed mucosa.
How is surgery performed ?
Surgery can be performed under general or peridural ansethesia. The classic surgical technique involves the resection of haemorrhoids grouped in 3-4 bundles and ligation of vessels at their base. Patients are discharged the following day and instructed to take painkillers, anti-inflammatory drugs and laxatives. Anal hygiene is done with a soft sponge and lukewarm water. Healing of the surgical wounds is complete after 3-4 weeks only and slight bleeding or mild purulent discharge is to be expected during that period. Pain can be rather vivid during the initial 10 days, usually requiring the patient to be on work leave.
 |
|
|
|
FIG: Haemorrhoids |
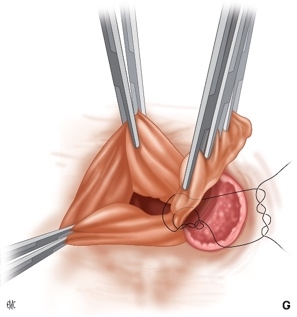
FIG: Bundle ligation |
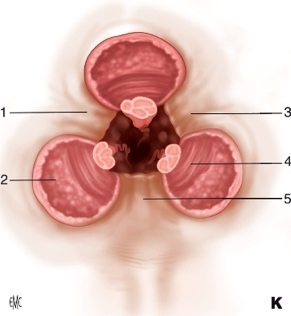
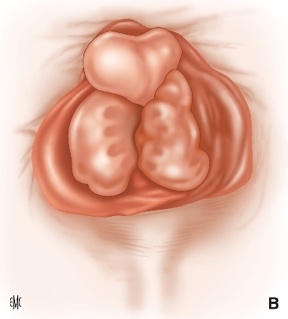
FIG: Classical haemorrhoidectomy in 3 bundles. Source : D Brachet,E Lermite,JP Arnaud Traitement chirurgical de la maladie hémorroïdaire EMC-Techniques chirurgicales-Appareil digestif 2012 ;7(2) :1-15 Article 40-685 |
Stapled haemorrhoidectomy: an alternative
A novel method has gained popularity because, unlike the above-mentioned technique, it does not leave open wounds and the attendant prolonged healing period. Using a circular stapler introduced through the anus the hemorrhoidal vessels are ligated and resected along with a 2-3cm cylinder of rectal lining. The resulting upward traction repositions the prolapsed anal mucosa within the anal canal. This technique is usually associated with less pain, minor bleeding and no purulent discharge, making it more comfortable. There is no wound care postoperatively.
 |
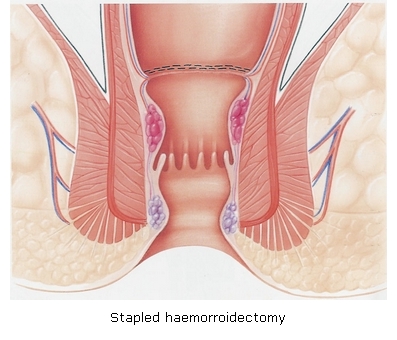 |
Figures courtesy of Johnson and Johnson.
Dr Serge Landen - www.drlanden.be